Most people with allergies will be very familiar with how and when they happen and what they feel like. However let us start the story again and quickly move to a re-think that may better fit with natural home measures.
Briefly, allergies are heightened immune system responses (‘hypersensitivity reactions’) to substances (allergens) that are typically harmless to most people. Allergens come in different forms, with different types of reaction.
- Environmental: caused by pollen, dust mites, mould, and pet hair.
- Dietary: acute reactions to foods like peanuts, tree nuts and shellfish, and also the consequence of more obscure ‘masked food allergies’ to proteins in foods like milk, wheat and eggs.
- Insects: reactions to stings from bees, wasps, or other insects.
- Medication: reactions to certain medicines.
We will explore these in future posts. When someone with allergies comes into contact with an allergen, the following occur:
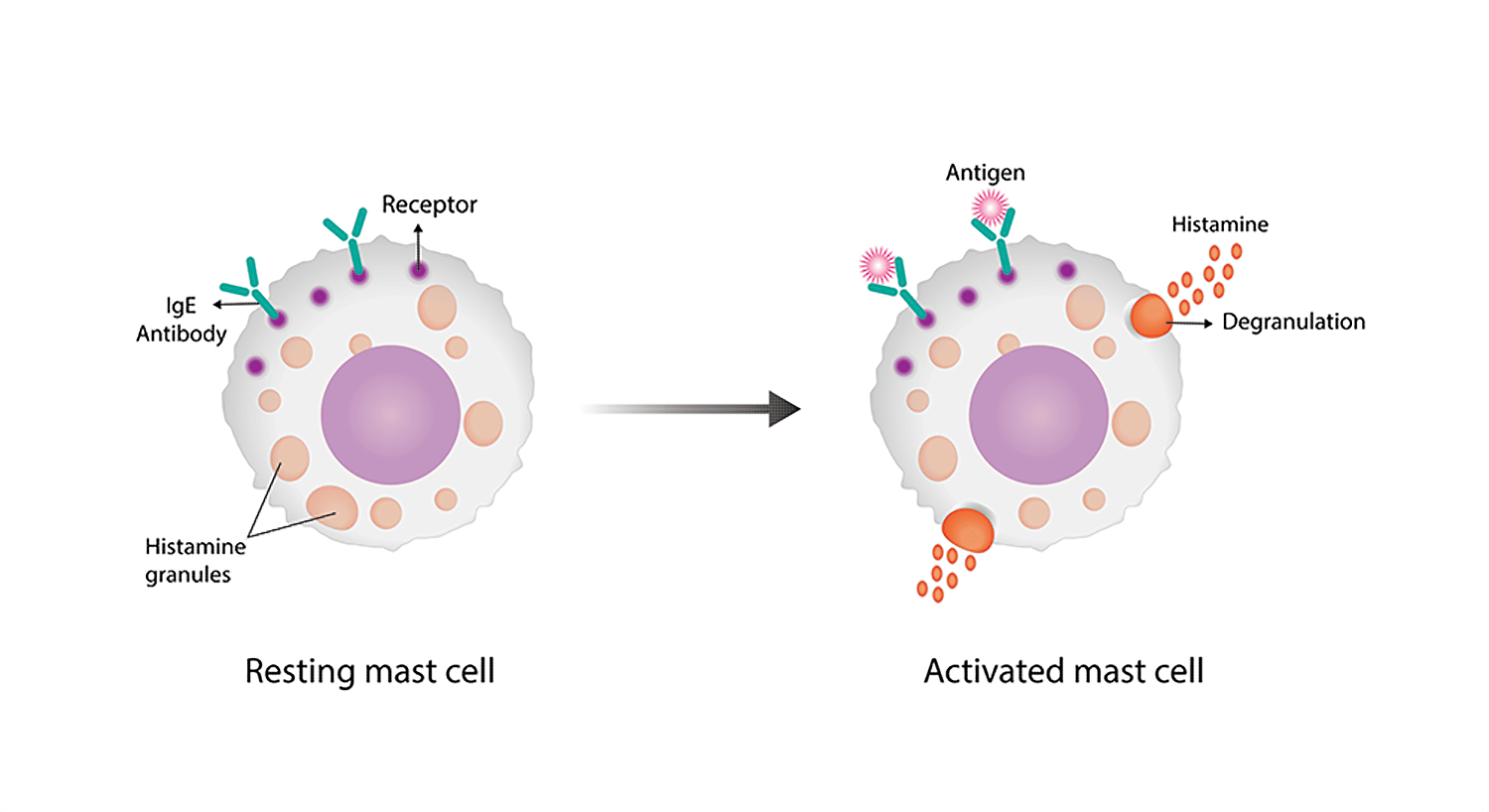
Sensitisation. On the first encounter, their immune system may mistakenly identify the allergen as a threat. In the case of overt allergic reactions in the airways and other surfaces it produces a special type of antibody, immunoglobulin E (IgE) specific to that allergen.
IgEs are produced by short-lived antibody-producing B-cells and are mostly attached to specific white blood cells: mast cells and basophils (see our Immune vanguard post). People prone to allergies may have inherited a tendency to produce more IgEs and or express them more on these cells. IgE production is a complex process regulated by various inflammatory mediators (cytokines), genetic factors and cellular mechanisms. It is known for example that one cytokine (IL-4) promotes IgE synthesis, while another (IFN-gamma) inhibits it. In other words, there may be wider inflammatory factors that could vary the IgE levels and thus the extent of any allergies.
Allergic reaction. On later exposures, the allergen binds to the IgE antibodies on mast cell / basophil surfaces. This activates the cells, leading to the release of cytokines such as
- Histamine: causing itching, swelling, and mucus production.
- Leukotrienes: contributing to inflammation and spasm of airways, leading to asthmatic symptoms.
- Prostaglandins: part of any inflammatory response causing pain and fever.
The allergic response
Symptoms are either local or systemic.
- Local symptoms: sneezing, itching, and nasal congestion in the respiratory tract; eczema and hives where the allergen contacts the skin; various gut problems with food allergies.
- Systemic reactions: food allergies may be linked to a wide range of mysterious symptoms around the body. In severe cases, allergens may lead to widespread release of cytokines that can lead to life-threatening symptoms: anaphylaxis, including difficulty breathing, rapid drop in blood pressure, and shock.
- Repeated exposure can lead to chronic inflammation in affected areas, resulting in conditions like allergic rhinitis (eg hayfever), asthma, or eczema.
General allergy management strategies. The most effective way to manage allergies is to avoid known allergens.
- Keep windows closed during high pollen seasons.
- Wash bedding regularly and consider sealing mattresses and covering or regularly replacing pillows.
- Intensively vacuum bedrooms and other rooms (with high-spec filter cleaners if possible) to minimize dust mites, pet hairs and other dust allergens.
- Maintain a clean and dry home as far as possible to reduce mould.
- Use air filters or masks where necessary to reduce exposure to pollen and dust.
- Shower and change clothes after being outdoors during pollen season.
- Avoid long exposure to heavy traffic areas (diesel fumes are particular stimulants of IgE production); if driving through congested roads switch off the car’s air intake and close windows to reduce exacerbating pollutants.
- Avoid smoke, smoking and other pollutants.
- Consider dietary adjustments for food allergies, including reading labels carefully.
- Check on any prescriptions or other medicines which may be associated with exacerbating allergic reactions.
Conventional medical treatments. The following may be necessary to manage symptoms and even save lives.
- Antihistamines: Help relieve sneezing, itching, and runny nose.
- Decongestants: Reduce nasal congestion.
- Nasal corticosteroids: Decrease inflammation in the nasal passages.
- Epinephrine auto-injectors: for severe allergic reactions including anaphylaxis. These may be life-saving and should always be carried if there is a risk of such a reaction.
- Immunotherapy: gradual exposure to allergens can help desensitize the immune response over time.
The hygiene hypothesis. There is increasing evidence that a lack of early childhood exposure to infectious agents and parasites increases susceptibility to allergic diseases and autoimmune conditions. This can be the result of modern hygiene practices, such as increased sanitation, reduced exposure to germs, and smaller family sizes. For example children raised in rural environments, where they have more exposure to animals and the outdoors, those in larger families and with more pets all tend to have lower rates of allergies. Essentially, this hypothesis suggests that our immune systems need some level of “training” through exposure to a variety of microbes to develop properly and differentiate between harmful and harmless substances. Although it may be thought that this will be difficult to correct after the event, there is an immunotherapy case for gentle ‘exposure to dirt’ even later in life: more outdoor activities and less reliance on home disinfectants for example, as long as these do not also provoke more allergic trouble.
As we saw earlier, people prone to allergies may have inherited a tendency to express more IgEs on their relevant white blood cells. There is a possible evolutionary value in this. IgEs are the body’s main assault weapon against worm and parasitic infestations, so these people would have been better adapted in the past and in areas where such infestations are common. There is recent evidence that even now they may protect against some cancers.
Natural approaches to managing allergies. There are few reliable plant remedies or other natural treatments that can compete directly with conventional medicines and it is better to see them doing a different job. Their role is to reduce reliance on pharmaceuticals rather than replace them. The aim is to help shift the body’s responses to allergens so they become less distressing.
We will wrap these up in the last article of this section, after reviewing particular allergic conditions in the following posts. Before we finish we should mention a related but distinct problem.

Chemical Sensitivities. Many people find household and industrial solvent fumes can set off symptoms like headaches or breathing difficulties. These are sometimes thought of as allergies although mechanisms are different. Multiple Chemical Sensitivity (MCS) is a distressing exacerbation of such reactions: many organ systems and functions can be affected, with symptoms including fatigue, headaches, lack of concentration, and memory loss. Often tests in MCA are frustrating as they do not identify any mechanisms.
One explanation however is that MCS, like allergies, does result from a form of immunologic dysfunction, in this case caused by inhalation of chemical fumes, leading to sensitivities to other agents. A recent elaboration is that MCS arises out of a neurologic dysfunction, in which inhaled chemicals travel along the olfactory nerve to the brain, causing neurotoxic effects and mood alterations. Anxiety, depression and panic disorders are common in MCS and some doctors consider them as partial causes of the problem. The olfactory route provides a direct cause of psychological symptoms.
Directly effective natural treatments for MCS are elusive although anything that can reduce the anxiety and exhaustion that most often attends the condition is likely to be helpful.


Recent Comments